-
Type:
EC eCQMs - Eligible Clinicians
-
Resolution: Answered
-
Priority:
Highest
-
Component/s: None
-
None
-
-
CMS0002v15
-
CMS0002v14
Hello,
I'm writing to get clarification in reference to resolution/comment posted on CQM-8251.
The question was for CMS2, regarding the outcome for the scenarios with multiple providers within a shared EMR.
Scenario 3:
Provider Sam has an encounter in January and no screening.
Provider John has an encounter and Positive screening on 1st of March.
Provider Trace has an encounter on 5th March and no screening.
Provider Kris has an encounter and does the follow-up on 15th March.
Provider Mary has an encounter in December and no screening.
–
Clarifying that in above Scenario3, the encounter on March15th is evaluating the screening findings. Screening was done on 3/1(which is within 14days prior to the 3/15 encounter). And followup is done on same day of the encounter 3/15.
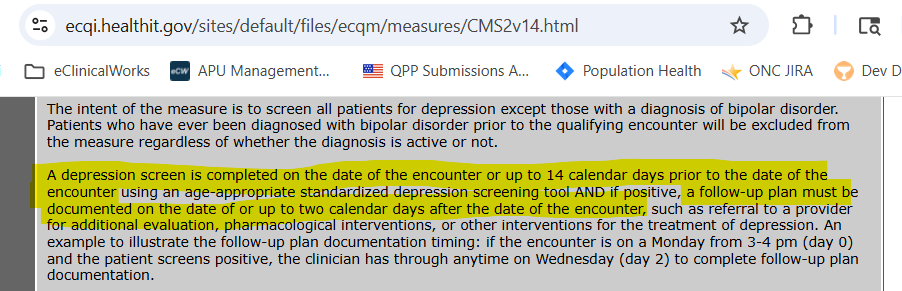
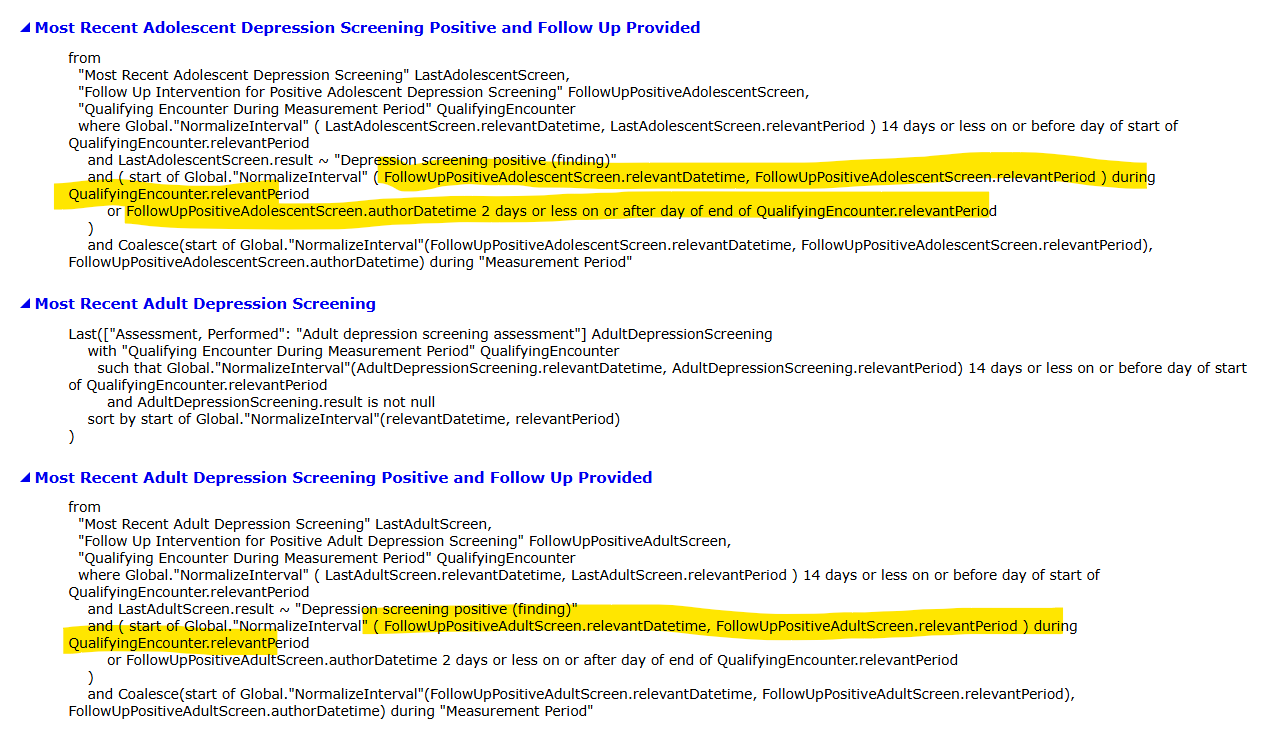
Per Measure Guidance :
"A depression screen(3/1) is completed on the date of the encounter or up to 14 calendar days prior to the date of the encounter(3/15) using an age-appropriate standardized depression screening tool AND if positive, a follow-up plan must be documented on the date(3/15) of or up to two calendar days after the date of the encounter(3/17)" .
Question1: With above scenario clarification and as per measure guidance, For Scenario3, would still all providers be Numerator NOT MET? Or Numerator MET? or if it differs for each provider, could you please mention the outcome for each?
Question2: If its still not MET, could you please explain in what situation is this 14day look back timeframe from an encounter and followup wthin 2days FROM the encounter is applied. And why is it not applicable here?
Per measure guidance and measure specifications(screenshots attached below), followup is calculated from the encounter, and not the screening. Please confirm.
Thank you for addressing our questions.