-
EC eCQMs - Eligible Clinicians
-
Resolution: Answered
-
Critical
-
None
-
None
-
Nancy Smith
-
7176808500
-
CureMD
-
-
CMS0002v11
-
It is required for UDS Reporting by the client.
https://ecqi.healthit.gov/sites/default/files/ecqm/measures/CMS2v11.html
In this HTML file, there are two LOINC codes mentioned that are used for Adult Depression screening assessment and Adolescent depression screening assessment
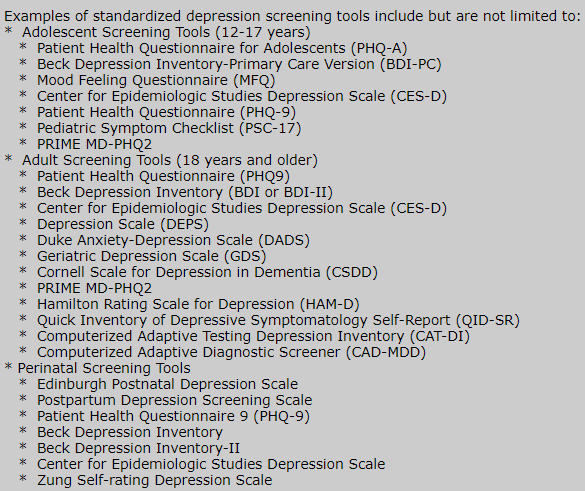
Is it possible that we link the codes, 73831-0 and 73832-9 to all the screening tools for depression mentioned under the below headings in the HTML file:
- Adolescent Screening Tools
- Adult Screening Tools