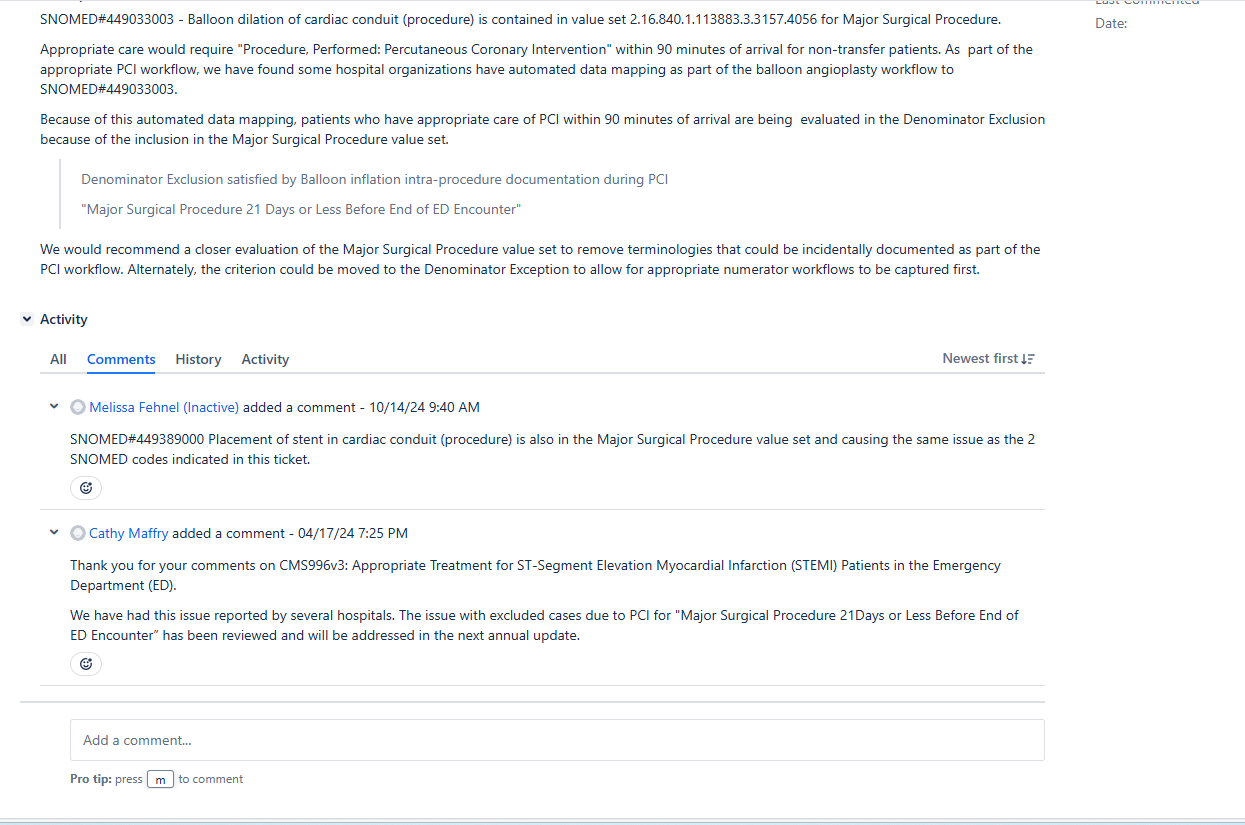
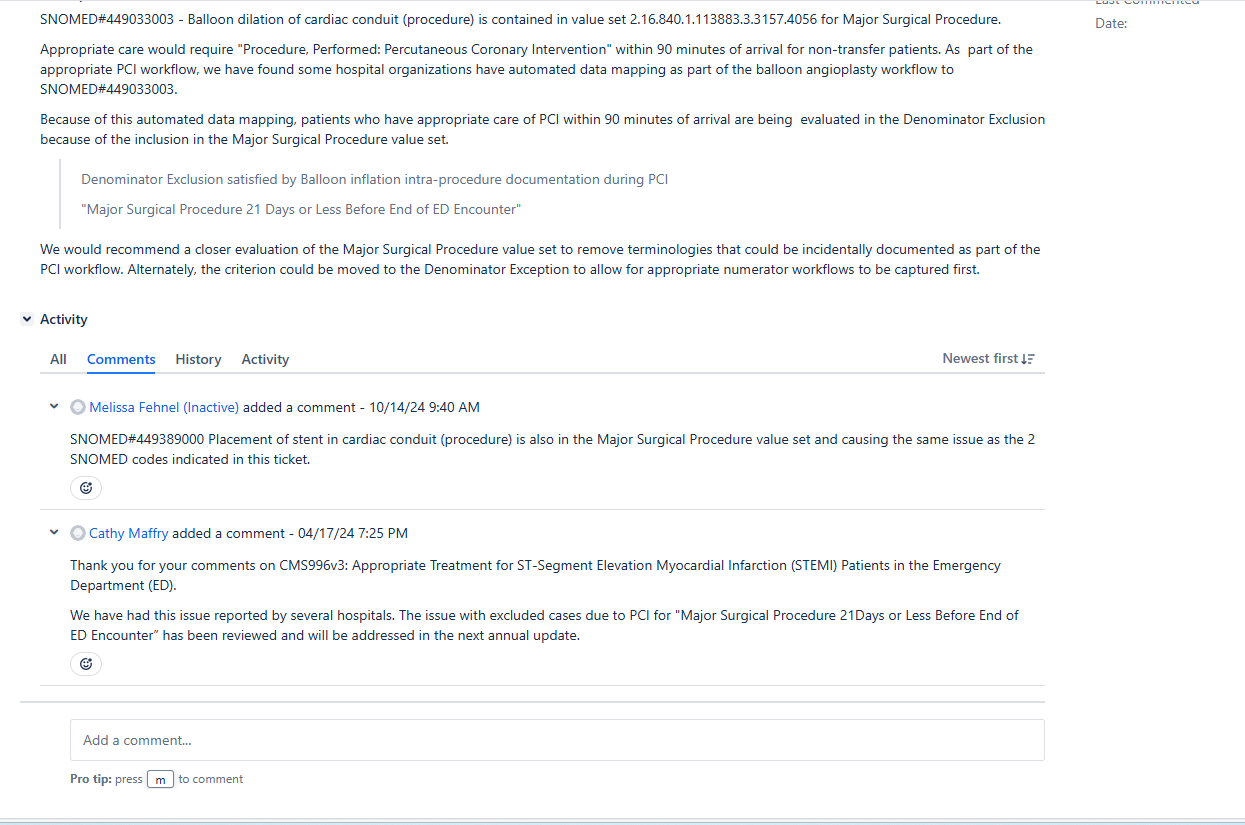
Thank you for your inquiry regarding CMS996v5, Appropriate Treatment for ST-Segment Elevation Myocardial Infarction (STEMI) Patients in the Emergency Department (ED). The measure captures the percentage of ED encounters for patients 18 years and older with a diagnosis of STEMI that received appropriate treatment, defined as fibrinolytic therapy within 30 minutes of ED arrival, percutaneous coronary intervention (PCI) within 90 minutes of ED arrival, or discharge to acute care within 45 minutes of ED arrival. The measure excludes major surgeries that occur 21 days or less before the start of the ED encounter or that start during the ED encounter using the Major Surgical Procedure value set (OID: 2.16.840.1.113883.3.3157.4056). The measure’s value sets were recently updated in Version 6 of the measure for the 2026 reporting period. Updated measure specifications have been posted to the eCQI Resource Center:
https://ecqi.healthit.gov/ecqm/hosp-outpt/2026/cms0996v6?qt-tabs_measure=measure-information. During this update, we removed PCI codes from the Major Surgical Procedure value set, so that STEMI patients who received PCI within 90 minutes of ED arrival would not inadvertently be excluded from the measure. Along those lines, we agree with your comment about removing any additional codes that indicate percutaneous coronary intervention since that is the procedure we are assessing. We are unclear if intervention to cardiac conduit (e.g., valve conduit, etc.) is happening with high frequency alongside STEMI, but please let us know if we are misunderstanding how cases are inadvertently being excluded from your facility. We wonder if this conduit code is being used for coronary bypass grafts. Value sets are updated annually, and we may consider removing additional codes from the Major Surgical Procedure value set in the future.
Hosp Outpt eCQMs - Hospital Outpatient eCQMs
Moderate