-
Type:
EC eCQMs - Eligible Clinicians
-
Resolution: Answered
-
Priority:
Moderate
-
Component/s: None
-
None
-
Sharanya
-
-
CMS0022v11, CMS0069v11, CMS0143v11
-
CMS0022v10, CMS0069v10
-
High. Telehealth exclusion is important to accurately evaluate the patients for measure eligibility/satisfaction
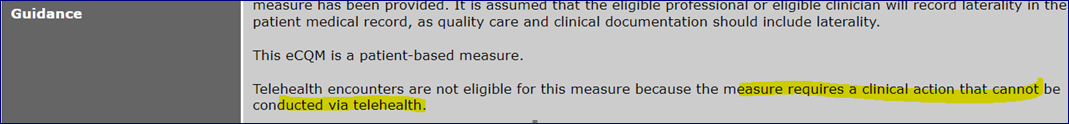
This is regarding the Telehealth exclusion for the 3 eCQMs wherein according to the guidance section, it states Clinical actions cannot be done via telehealth and hence not eligible.
In CMS69v11 (https://ecqi.healthit.gov/sites/default/files/ecqm/measures/CMS69v11.html), only the Denominator definition states telehealth encounters are ineligible as identified by a new "virtual" class parameter. The CMS69v11 numerator states BMI and the follow-up can be placed anytime during the measurement period.
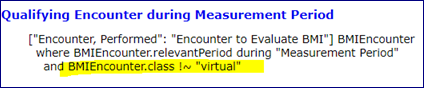
However, for the Numerator part, ie., BMI recorded or follow-up placed, there is no relation to the telehealth encounter.
Say for example -
- if a patient has a 1st encounter marked by a telehealth class (modifier), dated Jan 10th, then it is not eligible for the measure on the first instance.
For the same patient, another valid encounter dated July 1st is faced without any telehealth class, then this particular encounter will be eligible and measure qualifies.
If a BMI of normal value is recorded on the date of telehealth ir., Jan 10th, will this BMI be counted for the numerator evaluation and satisfy the measure?
- If a patient has a 1st encounter billed normally with a valid encounter code - dated Jan 20th and BMI is recorded on Jan 22nd. Say, another encounter is scheduled as a telehealth dated Jan 30th and a follow-up order is placed on the same day 30th Jan, will this be still counted for the numerator as pass?
As the CMS69v11 CQL definition has no clear indication of any conjunction of telehealth and BMI or follow-up intervention.
Kindly clarify.